What is Trauma and How Does Trauma Impact You?
What is trauma, and why is it a big deal? If you’ve wondered this, you’re not alone. This blog will explain what trauma is and how it impacts your emotions, thoughts, brain, and body—now and in the long term. If you are interested in the research you can read more in the hyperlinks throughout the blog.
What is Trauma?
Traditionally trauma was defined by, “Exposure to actual or threatened death, serious injury, or sexual violence (American Psychiatric Association, 2013).” Most people consider these events traumatic and understand if you have intense reactions such as fear and helplessness after experiencing them.
Trauma can also be, “An emotional wound or shock that creates substantial, lasting damage to the psychological development of a person, often leading to neurosis” (Houghton Mifflin Company, 1996). In other words an event hurts you badly and that pain stays with you, impacting the way you think and feel.
I like the definition two trauma researchers offered: “Events can be disturbing because of their personal significance, such as overhearing a passing remark that you are unattractive, getting a failing grade in school, or having a pet run away (Shapiro and Forrest, 1997).” In other words your individual, subjective experience of an event determines if that event is traumatic to you.
Societal norms and gender roles can be traumatizing
Sometimes trauma can be a condition instead of one specific event. Societal norms, gender roles, and the normalizing of abuse in society may traumatize you (Kesgin & Hashemipour, 2020) (Giller, 1999) (Falck, Frisen, Dhejne, & Armaund, 2021).
There are many events that might be traumatizing. What makes it traumatic for you is one of two things: 1) you experience the event as a threat to yourself in some way, or 2) your capacity to integrate your emotional experience is overwhelmed (Giller, 1999). We’ll talk more about this later.
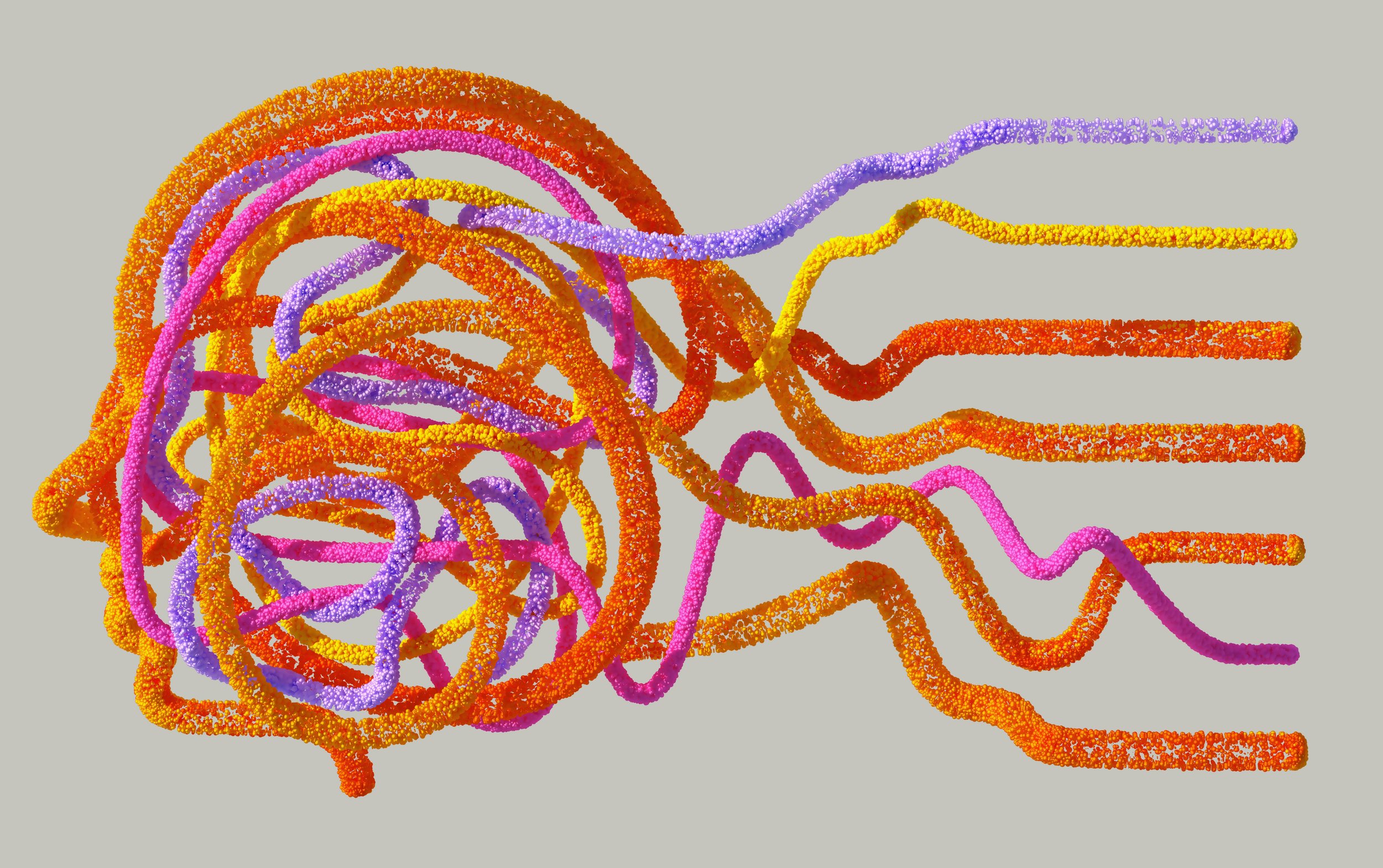
How Does Trauma Impact You?
So, what happens when you experience trauma? Trauma impacts your emotions, thoughts, brain, and body. When you don’t resolve the trauma there are serious, long-term consequences.
Emotional Impact
Emotionally speaking, you become dysregulated. Your emotions become more labile, popping from one feeling to the next. First anxiety, then suddenly irritability, leading to an angry outburst. It can start to feel lonely, like other people don’t really understand what you are going through. You may feel on guard and suspicious, preparing for something bad to happen.
Sometimes trauma creates dissociation—when you experience of being numb or detached from your own thoughts and body, or the sense that your experiences are not real. Things may seem dreamlike or distorted. If you experience these feelings, they may be related to traumas that you have encountered.
Impact on Cognition
Thoughts can change dramatically in the wake of trauma. You may find you cannot stop thinking about what happened, even when you try to avoid those thoughts. It becomes hard to focus or think clearly. Your view of yourself and others may shift, becoming more pessimistic. You are more likely to think about upsetting memories and ruminate on upsetting ideas. Over time this can impact the way that you think about the world and how you interact with everyone around you. But it is not just your psychosocial patterns that change.
Immediate Neurological Impact
Trauma alters your brain (Solomon & Heide, 2005). Immediately after a traumatic incident you experience a shift in your endocrine system, a rush of norepinephrine and epinephrine that jolt your system. Activation of the Hypothalamic-Pituitary-Adrenal system sends cortisol into the blood and you develop hypervigilance and a startle response. You are ready to fight or flee from danger! Over time, stress shifts these systems to impact daily hormone levels, metabolism, and neurophysiology. You can read the science-y stuff here!
Memory Storage is Impacted
This part is science-y, but it’s important. During typical memory storage your brain first puts the memory in the limbic system, a structure that processes emotions and memory. The limbic system consists of several different parts including (but not limited to) the hippocampus, amygdala, and hypothalamus. For a in-depth video tutorial on the neural anatomy of the limbic system, click here.
The amygdala is the center of emotions. During fairly emotionally neutral events the amygdala processes and attaches emotional content to memories while the hippocampus processes cognitive aspects. Once you’ve processed what happened, aspects of those memories are relocated to the neocortex for long-term storage. It’s sort of like putting data into a filing system. You figure out how you felt, what happened, organize and time-stamp the information, then file it away in the neocortex so you can reference it later.
When an event is more upsetting, like that stressful interaction with your family, it needs to process longer, so it lingers in the limbic system. The way you can get it out is to talk about, think about, and sometimes dream about what happened. This helps your brain consolidate the information as long term memory—in the neocortex filing system.
Thinking, talking, and dreaming helps consolidate emotional memory
During trauma your brain becomes overwhelmed and fails to process the experience. The memory is left, stuck in the limbic system triggering intense emotions (fear, anxiety), frightening thoughts, vivid images of the trauma, nightmares, and can even generate body sensations such as sounds or smells.
Your hypothalamus normally maintains homeostasis of hormones like a thermostat; However, the trauma triggers the amygdala, which sends a distress signal the hypothalamus, which in turn activates the sympathetic nervous system. Just by thinking about this distressing memory, which is stuck in the limbic system, your body reacts as though the event is happening now. The sympathetic nervous system prepares your body for fighting or fleeing!
Trauma gets you ready to fight or flee
Immediate Impact on Your Body
Your eyelids open, pupils dilate, sweat glands are stimulated, blood flow increases to your large muscle groups (like legs and arms), which means blood flow diminishes everywhere else (like your stomach and head), heart rate increases, your lung’s bronchial tubes open, and digestive system secretions are inhibited. You are ready to swing fists and pump your legs! But you may also have a stomach ache, lots of intestinal distress, muscle aches and cramps, dizziness, and a headache.
Dilated pupils
Your body becomes incredibly stressed, but there is nothing to actually fight or flee from. Instead, all of those chemicals just sit in your system, causing anxiety, panic, irritability, and anger. Thinking about the memory causes you to re-live traumas and feel an emotional and physical rollercoaster. So, you avoid the memory. Refusing to think about or process the memory means those memories are left stuck in the limbic system to continue wreaking havoc on emotions and physiology. It becomes a brutal cycle and has a cumulative, harmful impact on the body.
Long Term Impact on Your Body
Trauma damages your body and is associated with poor long-term health. Allostatic load refers to the compounded damages these chemicals and physical changes have on your body. High allostatic load correlates to significantly worse health, increased functional limitations, increased rates of diabetes, and increased rates of heart attacks (Monnat & Chandler, 2015). Traumatic stress is linked to hypertension (Kibler, Joshi, & Ma, 2009), increased heart disease, cancer, stroke, and mortality (Chae, et al., 2015), and consistently poor immune system response (Solomon & Heide, 2005). Allostatic load may trigger chronic musculoskeletal pain, persistent pain, and be related to the development of conditions such as fibromyalgia, irritable bowel syndrome, and chronic fatigue (McFarlane, 2010). These are definitely not good for you.
What You Can Do
Now that you know what trauma is and how it impacts your emotions, thoughts, brain, and body, what can you do about it? The good news is you’ve already started the first step—gathering information. Now you can take action. You can reduce the sources of trauma in your life and begin to process your trauma experiences.
You can try processing your trauma on your own. Another option is to find a good trauma therapist to support you. If you are interested in what trauma therapy looks like and how it can help you, stay tuned for my next blog. If you want more information, feel free to check out the rest of my website. You can also contact me to schedule a consultation.
References
American Psychiatric Association. (2013). American Psychiatric Association: Diagnostic and Statistical Manual of Mental Disorders, Fifth Edition. Arlington, VA: American Psychiatric Association.
Chae, D. H., Clouston, S., Hatzenbuehler, M. L., Kramer, M. R., Cooper, H. L., Wilson, S. M., . . . Link, B. G. (2015). Association between an Internet-Based Measure of Area Racism and Black Mortality. PLOS ONE, 10(4).
D'Antoni, F. (2021). Brainspottingn Reduces Disturbance and Increases Heart Rate Variability Linked to Distressing Memories: A Piolot Study. Mediterranean Journal of Clinical Psychology, 9(3).
D'Antoni, F., Matiz, A., Fabbro, F., & Crescentini, C. (2022, January). Psychotherapeutic Techniques for Distressing Memories: A Comparative Study between EMDR, Brainspotting, and Body Scan Meditation. International Journal of Environmental Research and Public Health, 19(2).
Falck, F., Frisen, L., Dhejne, C., & Armaund, G. (2021). Undergoing Pregnancy and Childbirth as Trans Masculine in Sweeden: Experiencing and Dealing with Structural Discrimination, Gender Norms, and Microaggressions in Antenatal Care, Delivery, and Gender Clinics. International Journal of Transgender Health, 22(1-2), 42-53.
Giller, E. (1999). What is Psychological Trauma? 15, p. 2021. Sidran Institute.
Hildebrand, A., Grand, D., & Stemmler, M. (2017). Brainspotting - The Efficacy of a New Therapy Approach for the Treatment of Posstraumatic Stress Disorder in Comparison to Eye Movement Desensitization and Reprocessing. Mediterranean Jounral of Clinical Psychology, 5(1).
Houghton Mifflin Company. (1996). The American Heritage Dictionary of the English Language, Third Edition. Bostonm MA: Houghton Mifflin Company.
Kesgin, C. E., & Hashemipour, S. (2020). The Imposed Post-Traumatic Stress Disorder by Communities and Its Impact on Females: Being Woman in Turkey and Iran. Dakam's Humanities Studies, (pp. 49-58).
Kibler, J. L., Joshi, K., & Ma, M. (2009, February). Hypertension in Relation to Posttraumatic Stress Disorder and Depression in the US National Comorbidity Survey. Behavioral Medicine, 34(Winter), 125-131.
Masson, J., Bernoussi, A., & Moukouta, C. S. (2017). Brainspotting Therapy: About a Bataclan Victim. Global Journal of Health Science.
McFarlane, A. C. (2010, February). The Long-Term Costs of Traumatic Stress: Intertwined Physical and Psychological Consequences. World Psychiatry, 9(1), 3-10.
Monnat, S. M., & Chandler, R. F. (2015). Long Term Physical Health Consequences of Adverse Childhood Experiences. The Sociological Quarterly, 54(4), 723-752.
Shapiro, F., & Forrest, M. S. (1997). EMDR: The Breakthrough Therapy for Overcoming Anxiety, Stress, and Trauma. New York, NY: Basic Books.
Solomon, E. P., & Heide, K. M. (2005, January). The Biology of Trauma. Journal of Interpersonal Violence, 10(1), 51-60.